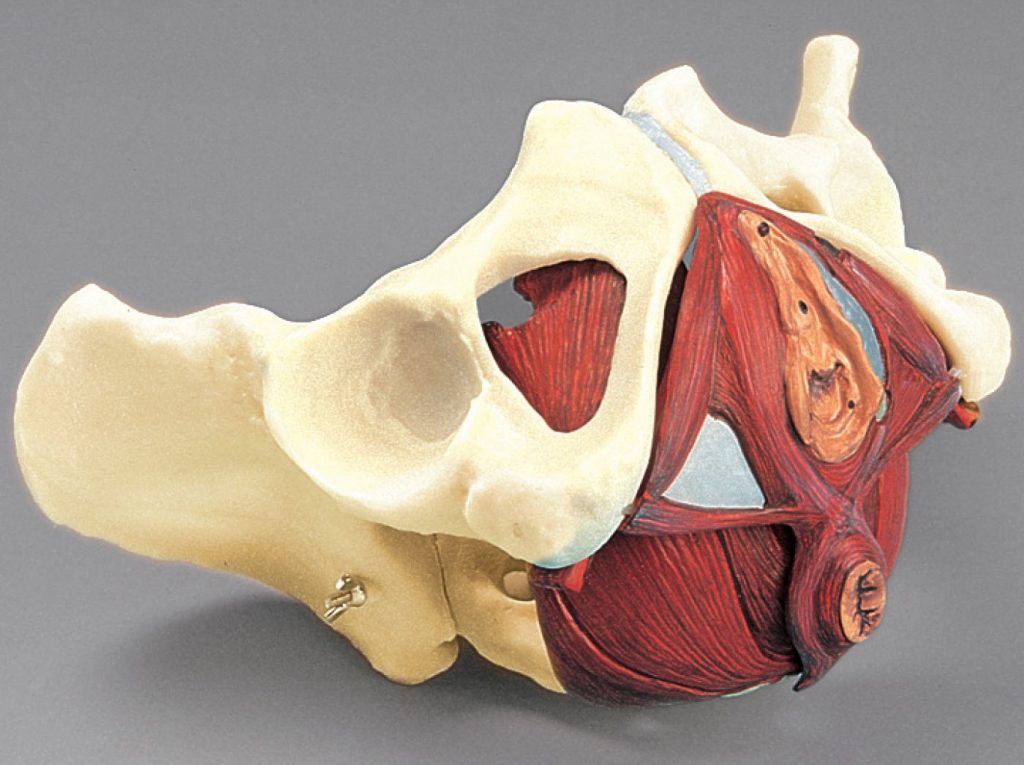
Pelvic Floor Physiotherapy is a first-line of defence against Incontinence and Pelvic Pain.
Pelvic Floor Dysfunction can be of two kinds:
- HYPOTONICITY (Weak pelvic floor muscles)Contributing to stress incontinence, urge incontinence and pelvic organ prolapse. Incontinence is NOT a normal part of aging neither is it normal after pregnancy
- HYPERTONICITY (Tight pelvic floor muscles):Contributing to Urinary and Fecal Urgency, Urge Incontinence, Chronic Pelvic Pain, Dyspareunia, Vaginismus, Vulvodynia, Pudendal Neuralgia, Interstitial Cystitis and Chronic Prostatitis
Who do I see for Pelvic floor dysfunction?
The Cochrane Collaboration (2010) concluded that specialized Physiotherapists should be the first line of defence for stress, urge and mixed incontinence in women. These physiotherapists have taken specialized training in pelvic floor rehabilitation. A Pelvic health Physiotherapist can also help with pre natal and post natal Physiotherapy.
Why do I need Pelvic Floor Physiotherapy?
If you experience pelvic pain, pain while urinating or having a bowel movement; painful intercourse, our highly experienced Pelvic health physiotherapist can help. Also if you are pregnant or recently delivered a baby, a Pelvic health physiotherapist can help correct the biomechanical changes that happen with pregnancy to hasten the healing process and help you get back to your routine in a safe manner.
How is Pelvic Floor Dysfunction diagnosed?
Specially trained doctors and physiotherapists diagnose pelvic floor dysfunction using internal and external “hands-on” techniques to evaluate the function of the pelvic floor muscles. Just like an orthopaedic assessment, a Pelvic health physiotherapist will evaluate the tone and strength of the pelvic floor muscles and their ability to function in tandem with the other muscles of the body.The bones and muscles of your lower back, hips and sacro-iliac joints will need to be assessed as well. As these joints can also stress your pelvic floor muscles.
<h5>What can I do to take care of myself?</h5>
Self-care is an important part of treatment. Avoid pushing or straining when urinating. And ask your health care provider about how to treat constipation. Relaxing the muscles in the pelvic floor area is important. Using methods such as warm baths twice daily can also be helpful.
Having a good posture keeps pressure off your bladder and pelvic organs. Stretching, relaxation and mindfulness techniques are also helpful.
Persistent pain education is an important part of treating pelvic floor dysfunction. Since the pelvic area is an area where we often hold our stress. Anxiety, stress and our attitudes and beliefs can perpetuate the pain in our pelvis. Understanding how our pain system works is an effective way of reducing the threat of constant pelvic floor dysfunction.